2020 has been a challenging year. COVID-19, longstanding racial inequities coming to a head, political divisions, and economic upheaval have collectively fomented into one of the most unique years I have witnessed in this nation across my lifespan. Daily reminders of these experiences figuratively and literally come crashing into our lives, and not a single life has escaped unaltered by these forces.
As a clinical psychologist, I have devoted the last two decades of my life attempting to understand how best to help individuals struggling to overcome various psychosocial challenges. At some point in all our lives we have weathered experiences of prolonged stress with elements of emotional helplessness and powerlessness commingled in varying degrees. The experienced intensity of the stressors, the age and length of time over which they occur, the type of relational resources we have around us during these periods, and our capacity to emotionally access them and experience them in a supportive manner often combine in inexplicable ways to surpass some invisible threshold, leading to an experience of psychological trauma.
Trauma ultimately exists outside the sphere of language and leaves an indelible imprint upon our psyches and bodies, powerfully shaping the unique array of physiological, emotional, behavioral, and relational patterns we then – often reactively and unconsciously – rely upon to “go on being.” In some sense, an adaptation or preservation has then occurred, though these adaptations oftentimes carry a defensive, inhibitive, self-destructive, or emotionally and relationally-destructive fragment within them. Thus, trauma becomes and remains a part of us.
While the current situational factors we are facing might very well have a traumatic impact upon any of us, what I’m more frequently observing in clinical work is how the present forces are, in tandem, serving as psychological triggers evoking or intensifying those unique patterns we historically internalized to weather the earlier storms of our lives: reactive isolation, compulsions, addictions, dissociation, shame, despair, self-hatred, or relational hegemony, to name a few. Thus, 2020 and all that it has ushered in become the grounds for a psychosocial regression and re-traumatization of sorts.
As a practitioner of the art of psychoanalytic psychotherapy, I spend my hours listening in a highly trained way to others: listening to language, thoughts, affect, sensations, experiences, dreams, parapraxis, defenses and resistances, psychosocial patterns layered within systems, experiences of objectification, exploitation, and oppression, and to various historic traumas endured and internalized; listening to what is unverbalized yet still communicated, listening to another’s experience of themselves and those in their lives, listening to their experience of me, listening to my self-experience as I tend to them, all as some further hint to the idiosyncratic nature and complexity of their struggles.
This listening, over a consistent and sustained period of time, informs how I aim to be and intervene in any given therapeutic hour with any individual so as to gradually introduce a sense of psychosocial healing and growth; to help another feel less alone, less anxious, less depressed, less overwhelmed, less painfully reactive, less compulsive, less confused, less afraid, less angry, less hurt, less empty, less numb or detached, less shame-ridden and self-hating. In essence, listening, being, reflecting, and intervening in a way with others so as to gradually help them become more aware of and free from the impact of situational, developmental, and relational traumas in their lives. All of which leads over time to a sense of more – more awareness, more engagement, more validation and security in self-experience, more emotional and relational freedom to choose and to act, more comfort being appropriately vulnerable in the right relationships, more emotionally connected, more hopeful, and a greater capacity to find pleasure and fulfillment in the simple beauties of life…
Art therapy is a form of expressive therapy that integrates art-making and the creative process with psychotherapy. This therapeutic method is rooted in the belief that individuals can enhance their mental health and personal awareness through the self-expression of art. Art therapy can be helpful in times where it is difficult to express emotions and thoughts in words. Sometimes our emotions can seem so overwhelming that we feel blocked and are unable to express ourselves verbally. The use of creative interventions can be beneficial when reflecting on past or current experiences, and processing trauma. Anyone can participate in this experience, as it does not require any particular skill or talent to take part in creative expression. Art Therapy can be used with individuals, families, couples, and groups, and is open to people of all ages.
The main focus is not entirely on the final image, as much as it is the process of creating art. Each art therapist has a slightly different approach. Whereas some sessions may be led with a specific prompt, other art therapy sessions may take on more of an open-studio approach. In the case where a prompt is given, this provides more direction and focus as to what the client wants to process during the session. An open-studio approach is typically one that does not follow a specific guideline or directive. There is no limit to materials, as art therapy can include painting, sculpting, drawing, collaging, coloring, or the use of multiple materials and found objects.
Our minds have a way of trying to protect us from pain and distress, which can sometimes lead to suppressed emotions and avoidance. Through creative expression, clients are able to gain personal insight, while confronting suppressed emotions and healing from past or current trauma. Some of our basic human needs and desires are to feel seen, heard, and understood without feeling judged or rejected. Visual processing helps you learn what it’s like to gain control and feel empowered by your own self-expression.
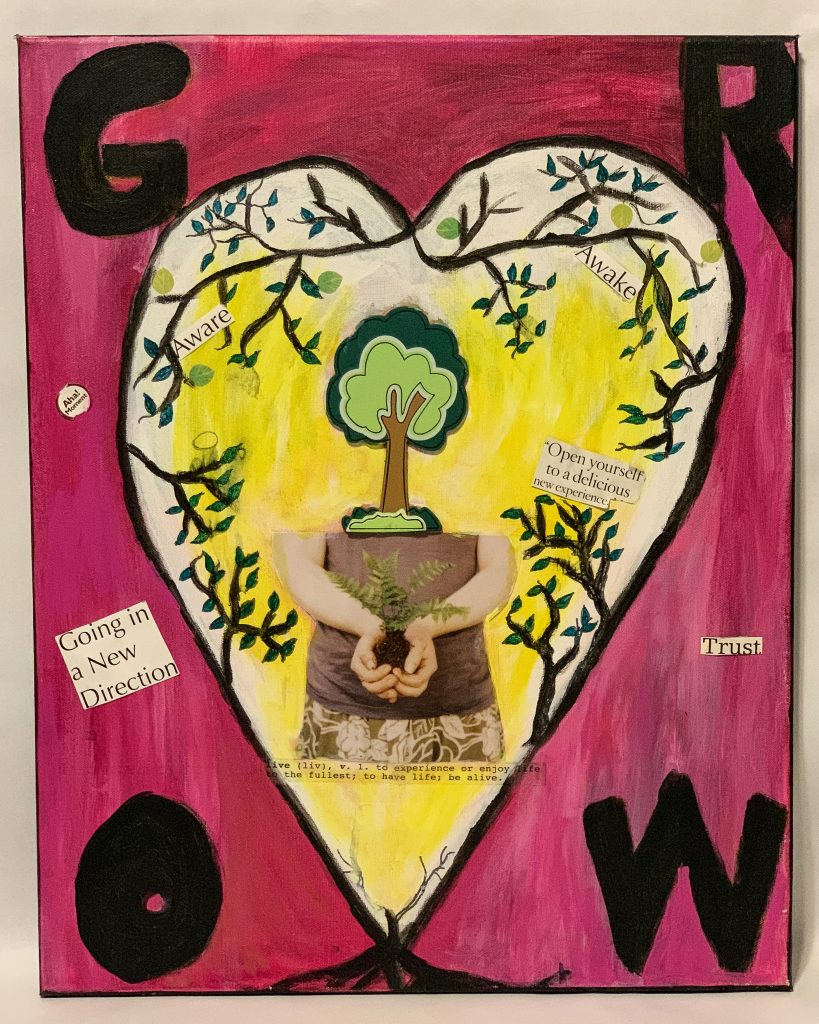
Pictured below are some examples of what art therapy looks like and how the process is used for personal reflection. The first image titled “Grow”, was created as a reflection of life changes and unexpected transitions. It is a normal instinct to try and plan and control the pieces of our lives. This individual used art to process unexpected life changes, and work through adjustment amidst a desire for control.
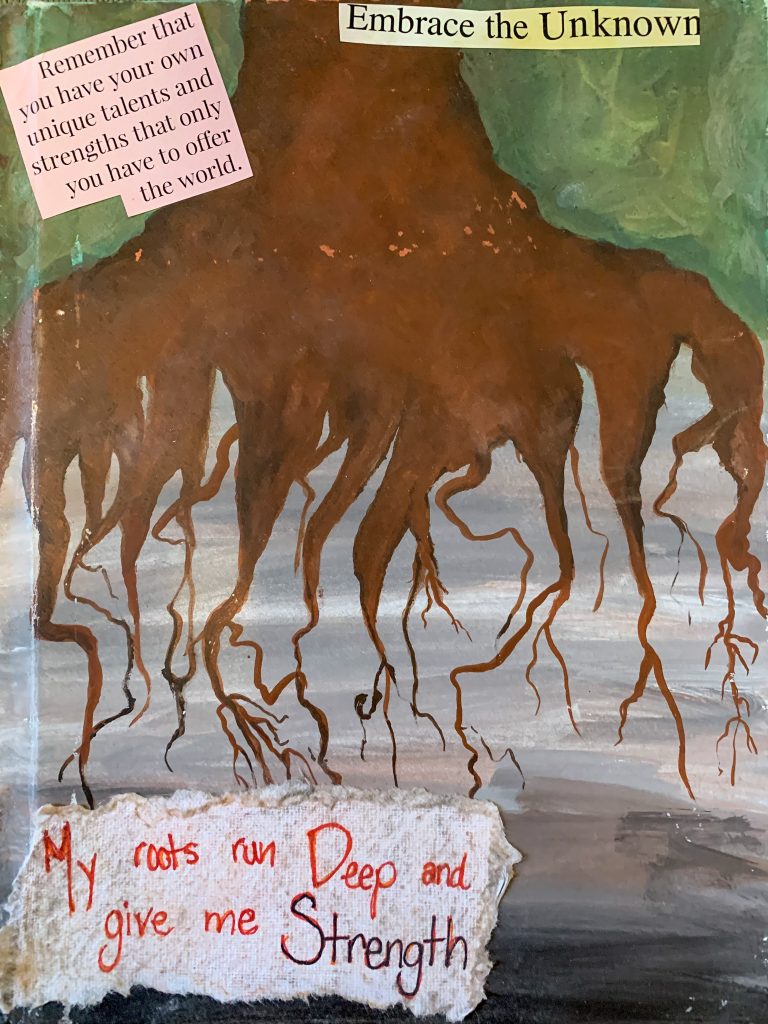
The second image titled “Roots”, was created out of a therapeutic prompt. The directive was to create an image that (to them) resembled strength and resiliency. This piece was created as a reflection of self-worth and self-acceptance.
The third image titled “Beauty in Brokenness”, is a piece that I actually did as a personal reflection of the impacts of COVID-19. I took a bare clay vase and broke it, glued the pieces back together, and stained the outside. The breaking of the vase is symbolic of the breakage and uprooting caused from the COVID-19 outbreak. I glued the pieces back together, and then stained the vase so all the cracks and missing pieces stood out. These cracks represent the scars, challenges, losses, and devastation caused from COVID-19. I wanted to make these visible and stand out as an encouragement to find the beauty and hope in healing. I used creative expression to process this on a personal and universal level. My concluding reflection was that the cracks are a part of us, but that they do not define us.
For more information and resources on art therapy, see these links below:
EMDR (Eye Movement Desensitization and Reprocessing) has been growing in popularity since its creation in the late 1980s as a leading treatment for traumas of all kinds. I often get raised eyebrows from people when I tell them what the acronym stands for. I get it; it’s long and doesn’t easily explain itself. But, hang in there, because it is truly incredible and unique.
EMDR provides understanding of trauma through the lens of how the brain responds to and stores traumatic experiences and the central nervous system’s activation in the body. Trauma seems to stunt the mind’s ability to healthfully process these events, therefore leaving them frozen in time with its various sensory components, emotions, body sensations, and disturbing beliefs. Anything that isn’t fully worked through can’t be properly cataloged away in your memory bank, so it is open to triggering high levels of distress in your present.
Sometimes triggers can be innocuous — a cabinet shutting a tad too loudly, the perfume/cologne of the person next to you, a song on the radio — but once your brain picks it up, it links directly to that unresolved trauma and turns on the alarm bells in your brain. Once that happens, your central nervous system may trigger a range of reactions such as a racing heart, body tension, sweaty palms, a panic attack, or feelings of dissociation.
Unresolved trauma trains the brain to constantly be on alert for threats of (real or perceived) danger and can create the feeling that your past is your present. EMDR was created to directly target unresolved trauma and provide a safe environment to navigate through it, make meaningful connections, and create new experiences of safety and security.
EMDR is unique from other forms of therapy in that while there is a talk-therapy component, it isn’t traditional talk therapy. Trauma is experienced on a spectrum. Some stories are easier to organize and talk about more than others. So, EMDR provides a way to connect to trauma in a structured way, that does not require vocalizing every detail of it.
So, what does it entail and look like? Once clients have the appropriate coping strategies they need to manage their symptoms and have mapped out the trauma they will tackle in therapy, one can begin the “R” of EMDR — reprocessing. This involves bilateral stimulation of your brain — through eye movements, tactile tappers, or audio tones — and free association. Subsequent to the long treatment name, this is usually where I get a second eyebrow raise.
Trauma stunts processing by deactivating the part of the brain that helps with language, organization, and meaning making. So, the bilateral stimulation of the brain while you focus on trauma keeps this part of your brain “online” to allow for your entire system to come to the table and work through the trauma. It also seems to accelerate the healing process faster than solely using talk-therapy. The free association component gives space for your mind to wander wherever it needs to within the trauma. The more you lean into the disorganization of the trauma, the brain finds a way to organize and resolve the distress.
EMDR is a great sole focus or adjunctive addition in therapy and can be applied to many presenting issues and levels of trauma. Once trauma has been resolved there is a rich opportunity for post-traumatic growth: a newly minted way of experiencing yourself and the world around you with a sense of empowerment, security, and confidence.
For additional information on EMDR, check out these helpful resources: